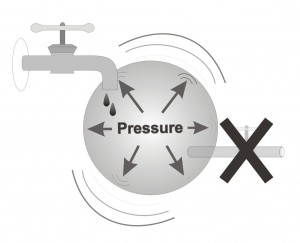
High Intraocular pressure – there is no doubt that high intraocular pressure is the greatest risk factor causing glaucoma and damage to the ocular nerve, yet, only less than half of the people with high intra-ocular pressure will suffer from glaucoma and about a quarter of the patients with glaucoma do not have high intra-ocular pressure. Therefore, high intra-ocular pressure is not the only cause of glaucoma.
Age- was shown to influence the development of high intra-ocular pressure, which in turn causes glaucoma . Intraocular pressure increases greatly after the age of 40 in those individuals susceptible to develop the disease. In general, with increasing age, various physiological functions such as strength, memory and flexibility deteriorate. Likewise, with aging the ability to drain the fluids out of the eye decreases, in parallel with a small decrease in the capacity to produce such fluid. Most often these two processes cancel each other and hence there is no net affect on the intra-ocular pressure. In some eyes the decrease in drainage capacity is much greater then the decrease in production, causing a significant rise in the intra-ocular pressure. The diminished capacity to drain the fluids of the eye effectively usually worsens with increasing age.
Family history- it has been shown statistically that some families have a greater incidence of glaucoma. Therefore, having relatives with glaucoma increases the risk of developing this eye disease. However, it is very common that in an entire family only one member has developed glaucoma. We believe that glaucoma has a strong genetic component, like many other chronic diseases. Hence, when one family member is diagnosed with glaucoma, his/her immediate (first degree) relatives, notably parents, brothers/sisters, and children, should consider being examined by an ophthalmologist, usually when reaching age 35 or 40. In cases that the affected individual has demonstrated the disease at an age younger than 40, all immediate family members should best be examined irrespective of age.
Ethnic background- research has shown that individuals of East-African origin are at greater risk of developing glaucoma. This is due to two reasons: Individuals of African origin may have higher intra-ocular pressure and tend to develop increased intra-ocular pressure at an earlier age when compared to individuals of European, Middle Eastern and Asian origin. In addition, a comparison of the damage inflicted on the ocular nerve at equal levels of Intra-ocular pressure in individuals of different origins has shown that individuals of African origin have a higher rate of damage found in their optic nerves. To date there is no evidence of a higher frequency of glaucoma among the Jewish population and there is no clear difference in the frequency among Jews of different origins.
Gender- women are at a slightly greater risk of developing open-angle glaucoma. On the other hand, it is important to bear in mind that women are at a much greater risk (2-3 times more then men) of developing closed-angle glaucoma. Hence, most cases of closed-angle glaucoma are found in women.
Myopia (short-sightedness)– even though there is no difference in intra-ocular pressure between near-sited, far-sited and individuals who don’t need glasses, it has been shown that among far-sited (hyperopic) individuals there is a much higher frequency of closed angle glaucoma. In addition, near-sited (myopic) individuals are more vulnerable to increased intra-ocular pressure. Therefore, a near-sited individual with high intra-ocular pressure is at a slightly greater danger of developing (or worsening of his/her) glaucoma then a far-sited or normal-sighted individual with the same level of intra-ocular pressure.
Impaired blood flow- individuals with impaired blood flow are perhaps at an increased risk of developing glaucoma. In addition, among glaucoma patients there is an increased number of individuals suffering from different complications associated with impaired blood flow such as migraine type headaches, high blood pressure, low blood pressure, impaired blood flow to the fingers and toes, diabetes, blood vessel related diseases, and heart diseases.
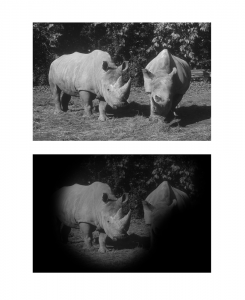
Summary and additional information Glaucoma is a common disease, mostly found above age 40 and with an increased frequency with increasing age. Statistics show that 2-4% of the population above age 40 may develop the disease and that 10% of the population above 90 actually has glaucoma. In addition, glaucoma is a disease that, more often then not, goes unnoticed. Therefore, it is not difficult to understand how even in developed countries such as the U.S.A and Israel for every diagnosed patient suffering from glaucoma there is another individual who has the disease, but has not yet been diagnosed.
For this reason it is recommended that individuals whose first-degree relatives are known to have glaucoma approach their ophthalmologist and obtain eye examinations routinely (perhaps once a year) after the age of 40. This examination will exclude glaucoma as well as other eye diseases that develop with age, such as cataract and retinal degeneration. Since the commencement of the Nation Health Law, all Israeli citizens are entitled to a free examination at their ophthalmologist through their Kupat-Cholim, their Health Maintenance Organization. It is not reasonable to expect all healthy Israeli citizens over the age of 40 with no complaints relating to their vision to approach their ophthalmologist for an eye examination (although we would certainly want this to happen), therefore, we will define who is at increased risk of developing glaucoma and should be encouraged to be routinely tested by their ophthalmologist.
The risk factors for developing glaucoma are primarily age and the existence of the disease in a first-degree relative. I recommend that any individual over the age of 40 with a family history of glaucoma to make an appointment with an ophthalmologist for a thorough eye examination in order to exclude glaucoma and other eye diseases. Other factors that slightly raise the chance of developing glaucoma include diabetes, high blood pressure, impaired thyroid function, myopia and prior eye surgery.
How often should an eye examination be performed? Well, my answer is as follows: the most important stage is to schedule the first appointment. This stage is the responsibility of the patient. Once the initial assessment has been performed the ophthalmologist may send the patient for further tests (if required) and recommend when the next examination should take place; according to the individual’s risk factors and any findings found during the actual eye examination.
In conclusion, it is important to remember that there are eye diseases that can be diagnosed and treated even before the patient feels any symptoms. Glaucoma is one of these diseases, in which it is crucial to diagnose it as soon as possible. While examined by your ophthalmologist, he/she will also check your eyes for the existence of cataracts, damage to the macula (the center of the retina) and early warning signs of any other eye diseases.