Why do I have very severe damage in one eye and in the other eye only “mild” glaucoma?
Glaucoma is a chronic disease which damages the optic nerve slowly and gradually during the course of many years and even decades. Even though it would make sense that the disease would damage both eyes equally, it is not necessarily so. Intraocular pressure is usually unequal between the two eyes, the more damaged eye having a higher pressure, and perhaps for a longer period of time. In many cases there are other differences between the two eyes: for example, medical treatment can have a better effect on one eye than the other. For this reason it is occasionally needed to treat each eye separately, according to the amount of damage and that eye’s response to medical treatment.
What is the difference between Glaucoma and increased intraocular pressure?
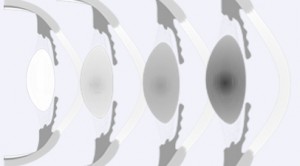
Glaucoma is a disease in which increased intraocular pressure damages the optic nerve and the visual field. Many people have increased intraocular pressure but do not suffer from glaucoma because their optic nerve is probably particularly strong and durable. We consider these people to be at risk of developing glaucoma in the future, and so they require regular follow up and sometimes, if the doctor finds it necessary, even treatment to reduce intraocular pressure, especially if it is particularly high. It is often difiicult to determine the best possible treatment for such patients (as they have intraocular pressure but had not yet developed glaucoma), as this treatment would need to be given regularly for the rest of their life. For this reason your doctor usually decides to give treatment only after collecting enough information to justify it.
I have been diagnosed with glaucoma: could I go blind?
There are patients, especially when first diagnosed, who express fear of their glaucoma becoming so severe, to the extent of blindness. First, it is important to understand that for a person who has glaucoma and is not receiving any treatment, there is a certain risk of going blind, but the course of the disease leading up to blindness even in untreated individuals is usually very long and gradual. On the other hand, patients receiving treatment are usually stable and do not have a substantial risk of going blind. There are some exceptions; some patients hold such a risk, but these are usually patients who have been diagnosed at a very late stage, when the disease has already damaged most of the optic nerve fibers, and who, in addition, suffer from an especially severe and aggressive form of glaucoma. Ordinarily, it is uncommon that a well-treated patient would become blind in one eye, and blindness in both eyes in such a patient is quite rare. There are many patients for which fear and anxiety caused by glaucoma are a bigger hindrance to their quality of living than the actual eye disease.
On the other hand it is important to mention that there is a group for which the risk of vision loss due to glaucoma is much higher. These are patients that had already lost one eye because of glaucoma. For them there is a risk of losing their vision in the second eye because of the same factors which caused the damage in the first eye. Patients in this group will usually be checked at a higher rate and receive more aggressive care in order to achieve low intraocular pressure, which would decrease to a minimum their risk due to glaucoma in their good eye. A patient in this group must be extremely meticulous about the treatment, revisiting the eye doctor and doing the tests they are referred to (such as visual-field tests).
One must remember that there are other reasons, besides glaucoma, which cause loss of vision (such as a retinal detachment, damage to the eye due to diabetes, damage to the cornea, injury, and more). It is important to emphasize the exception that patients who lost their vision in one eye due to other reasons (not glaucoma) are usually not at risk for vision loss due to glaucoma in their second eye.
Some patients withhold from living their life to the fullest (for example do not fly abroad, do not do normal exercise, do not have sexual relations, and so on) for no medical reason which has to do with their disease. If a patient is anxious about the possibility of losing their sight, it is important they share this with their doctor, in order to receive information about their condition, information which in most cases would have a soothing effect on the patient.
What is the optimal way to use eye drops?
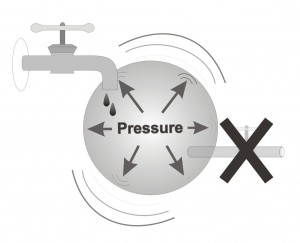
Correct use of eye drops is important so that they exert their full therapeutic effect. Many patients don’t know that it is possible to significantly improve the medicine’s efficiency by blocking the tear draining canal. The openings of the tear draining canal are on the upper and lower eyelids, a finger’s distance from both sides of the nose bridge, and they drain tears from the eye’s surface into the nasal cavity (that is why the nose “tears” when you cry). Drops that reach the nose are then absorbed into the blood, or are swallowed (that is the reason for the bitter taste that some patients sense after using eye drops).
The eye drops are absorbed into the eye by touching the surface, and the longer the drop stays on the eye’s surface the more efficient its absorption is. A large part of the drop could drain into the tear canal before it is fully absorbed into the eye, which lessens its effectiveness. It is possible to enlarge the part of the drop that comes in contact with the eye by blocking the tear canals, which is done by pressing on them lightly with your finger for 1 minute after placing each drop into the eye. This action does not only make the medicine more efficient by enlarging the amount of medicine which is absorbed into the eye, but also lessens the amount of the drop which drains into the nose, and so lessens the side effects to the rest of the body, which arise from the medicine being absorbed into the blood stream.
The correct way to use eye drops:
- Tilt your head backwards and look up. Pull your lower eyelid gently, to create a small pouch into which you can drop the eye drops. Because more than one drop might be dropped, you should have some tissues ready.
- After dropping the drop, close your eye gently. Try and avoid blinking, as that could push the drop into the tear canal and through it into the nose. It is also recommended not to close your eye very tightly, as that may cause the drop to be spilled from your eye onto your cheek. Closing your eyes gently will keep the drop and your eye in good contact and will allow maximal absorption of the medicine into the eye.
- Block the tear canal with your thumb for 1 minute. It is important to remember to close your eyes while lightly pressing on the tear canals’ openings. Closing the tear canal is important as those lead to the nasal cavity, where the drop can easily escape into the nose and from there pass into the blood stream.
- If you use more than one kind of drop in the same eye, you should wait 5 minutes between each kind, that is because the eye can only contain one drop at any given moment. Adding a second drop before the previous one has been completely absorbed would make the eye overflow, and the dirst drop would spill out of the eye.
It is important to bring your eye drops with you every time you visit your eye doctor, so he/she can accurately verify the eye drops you use, and see that there is no confusion as to the type of drops, the dosage, and the eye for which you use each bottle.
Remember:
1. Before using the drops wash your hands with soap.
2. Keep the medicine bottle clean and avoid touching the tip of the bottle.
3. After using the drops, close the bottle immediately. Do not wipe or wash the top end tip of the bottle.
Much more about the correct usage of eye drops is available at: 10 important tips for instilling eye drops.
What is the correct order to use my eye drops?
The order of using eye drop bottles doesn’t matter. What’s important is giving each drop enough time, about 5 minutes, to absorb. That is why a patient who is treated with different types of drops can use them in any order they want, but they should make sure they take a 5 minute break between each bottle. Exceptional are patients which use Gell eye drops, which are more viscous, hence it is recommended to use them last.
What do I do in case I forgot to take my medicine?
Don’t worry! Every patient might forget to take their drops once or twice. You should instill your drops when you recall you forgot them, and then continue normally. If you recalled it only around the time you’re supposed to take the next drop, don’t try to make up for it by instilling more than one drop, as that would be ineffective.
Is it dangerous to instill so many eye drops every day, for years?
When comparing the benefits of taking glaucoma drops, which are meant to prevent the irreversible damage that glaucoma has on vision, as compared to the damage which might be caused by the medicine’s side effects, it is quite clear that there is a significant advantage to using the drops. Only rarely do severe side effects show up, requiring the patient to stop taking the medication, and that is of course only after consulting your doctor and receiving his/her approval. In these cases too, it is usually possible to find an alternative drop, which does not lead to significant discomfort or side effects to that particular patient.
Are there medications that can cause glaucoma?
The answer is yes. Although usually glaucoma isn’t cause by taking medications or by any other action whatesoever performed by the patient, there are some rare cases in which glaucoma can be caused by taking certain medications. Among the medications which can cause glaucoma it is important to mention one, medications from the steroid family.
As a rule, steroids taken in the form of pills might cause cataract, and more rarely – glaucoma. These are cases in which the medicine is taken chronically, for long periods of time of months and years. In contrast, insome individuals, steroids tend to increase intraocular pressure significantly when taken as eye drops. Steroidal eye drops are given in cases of significant irratation to the eye, a severe inflammation or a severe allergy. In these cases the ophthalmologist usaully perscribes the medication for a limited period, which doesn’t extend past a few weeks. Patients who need these medications for longer periods will be under the supervision of their eye doctor, which will occasionaly measure their intraocular pressure, just to make sure that it has not risen. It should be noted that the elevation of intraocular pressure doesn’t have to be immediate, and could also appear a few months after starting the steriodal medication. That is why it is recommended not to take these kind of drops for a period longer than a few weeks without an eye doctor monitoring the patient. Pharmacists are also cautious about renewing such perscription over time, and might demand a new perscription from the eye doctor every time the patient comes to renew the medicine.
Despite all that has been said about steroidal drops, they are given freely and for long periods of time after glaucoma surgeries, to help keep the surgical opening patent for as long as possible. These drops are an important tool for the eye doctor after different surgeries, and particularly after glaucoma surgery.
There are some other medications which could worsen an existing glaucoma or increase intraocular pressure in healthy eyes, but these effects (except the effect of steroids that was mentioned) are rather rare.
I would like to ask my eye doctor to perform glaucoma surgery, to spare me the burden of having to use my eye drops for the rest of my life. What would be his answer?
Rarely does a patient come with this request to their eye doctor. Such a patient would have an attitude saying: “Let’s try and solve this problem once and for all and cure my glaucoma”. It is important to stress that every surgery has its risks, as rare as they may be, whereas in medicinal treatment these risks usually do not exist. For this reason the ophthalmologist would rather take care of the disease by medications if he thinks they will be enough to stop the progression of the disease and stabilize the patient. Usually only in those cases when medications do not sufficiently decrease introcular pressure, would the doctor recommend surgery. There are a few exceptions, for example patients who suffer from very high intraocular pressure, so high that it is clear to the doctor that only surgery could help in this case. Other examples for cases requiring immediate surgery are certain types of glaucoma which were proven to be sufficiently untreatable with medications alone.
Would the fact that I had cataract surgery in the past hinder my possibility to undergo successful glaucoma surgery?
Many patients over 60 suffer from cataract and glaucoma. In this situation there is an option that one eye would need cataract surgery, and in addition, sooner or later, that same eye would need glaucoma surgery. Some patients are concerned by the thought that their eye would go through more than one surgery, and the thought that one surgery could hinder the other surgery’s success. The answer is that it depends much on the order of surgeries, as well as on other characteristics of the condition. It is true that the more times you operate on the same eye, the later surgeries might become a little more complicated and require greater skill. More specifically, an eye that was operated on in the past with cataract could undergo glaucoma surgery with no added difficulties. When such surgeries are done in the opposite order (first glaucoma and then cataract), the situation is a little more complicated, since after glaucoma surgery was performed, every future surgery holds a small risk of harming the results of the previous glaucoma surgery. Due to this fact patients who went through glaucoma surgery in the past, and now need cataract surgery, need edded attention during the cataract surgery. It is important to remember that for the operating surgeon these are common occurances, since many patients undergo more than one surgery in the same eye. Your eye surgeon has the skill to perform these procedures in the best possible way and to carry out steps that will increase the chances of success.
How will glaucoma affect my quality of life?
The life of every person diagnosed with a chronic disease changes to some degree. Fortunately, in gluacoma, in most cases the disruption to every day life is minimal, almost without any hindrenace.
Despite that, there are a few areas which demand attention:
- It is necessary to be regularly examined by an eye doctor for many years (actually indefinitely), to pefrom tests as necessary and to take responsibility for the treatment.
- It is necessary to use medications (usually in the form of drops) routinely and regularly, and make sure that there is a sufficient supply of medications (so that you never run out).
- Sometimes there are side effects (usually mild ones) caused by the eye drops. Some might justify changing the medications.
- Any damage to vision, already present or should it develop in the future, might affect the patient’s life; in very severe cases it could force the patient to give up driving, and in rare cases it would be necessary to significantly adjust the life style to a state of very poor vision.
- Often (always) there are fears and concerns related to having been diagnosed with glaucoma, some rational and understandable, and some which could be significantly lessened by learning and reading a little more about the disease.
How should a patient newly diagnosed cope with this new situation? First, you can bring up problems and concerns during your visit with your eye doctor. Your doctor has enormous experience with many different kinds of patients, and most likely had already heard, many times, problems and concerns similar to yours, and hence could advise you on how to deal with the situation, and try and sooth your concerns. When your doctor perscribes you a certain medicine, it isn’t possible to know in advance its effect on any specific patient and what might be the side effects. However, after starting to take the medicine, if problems arise, your doctor can replace the medication, until finding the type of drops which will achieve the best care with as little or even no side effects. Last, any patient going on a long vacation, especially when travelling abroad, must make sure they have a sufficient supply of medications before leaving.