How will my eye doctor decide if I actually have glaucoma, or maybe not?
Glaucoma, in the vast majority of cases goes unnoticed, and hence, undiagnosed. Those suffering from this disease typically do not experience any pain or discomfort, and the visual field defects are not usually noticeable to the patient himself/herself. In contrast, during a routine eye examination your ophthalmologist can perform several specific tests to determine whether you have this disease. According to the results of these tests the doctor will let you know whether you suffering from glaucoma or whether there is need of further examinations. During this assessment process your ophthalmologist will question you about physical complaints you might have, about your medical background and any medications you might be taking. A thorough eye examination will then be performed, which may include the following:
 Visual acuity
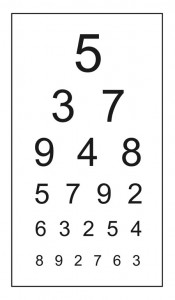
Visual acuity
this is a routine, but crucial, examination in which the patient is asked to read characters of decreasing size from a well lit wall chart, while one eye at a time is covered. Refractive problems (the need for glasses), such as myopia and astigmatism are one of the most common problems which can easily be diagnosed by this test and can be treated by prescribing glasses of the appropriate strength and prescription. Decreased visual acuity which cannot be fixed using glasses is attributed to eye diseases, which can be secondary to many different eye conditions, some treatable and some less so.
Examining the eye with a slit-lamp
during this test the patient is asked to place his/her face in a device somewhat resembling a microscope. During the examination, a narrow beam of light is projected from this device into the eye (hence the name – “slit lamp”). Using this device, the doctor, sitting across from the patient, can efficiently examine different parts of each eye such as the cornea, the iris, the lens, the vitreous and the retina, as well as the angle and the optic nerve head. This test enables the examiner to identify signs present in various eye diseases, and hence lead to the correct diagnosis. While diagnosing glaucoma, a thorough “slit-lamp” examination, performed by an experienced glaucoma specialist, can determine which type of glaucoma the patient has, as well as clues as to why did glaucoma develop in that particular eye and patient.


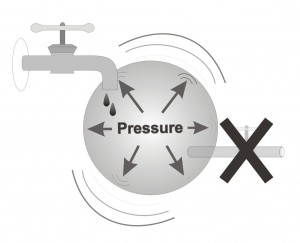
Measuring the intraocular pressure
this test is performed as part of the slit-lamp examination. In order to measure the pressure in the eye a drop of a yellow colored sedative (anesthetic drop) is applied to the eye rendering the external part of the eye (the surface of the eye) temporarily numb. This numbing usually lasts for around 20-30 minutes. A special instrument for measuring intra-ocular pressure (called a ‘tonometer’) is then brought towards the eye in order to take a pressure measurement. The intra-ocular pressure is evaluated in units of pressure also called ‘mmHg’ (i.e. ‘millimeters of mercury’)
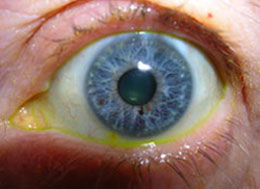

Examining the angle of the eye
sedation the external surface of the eye enables the ophthalmologist to examine the “angle” of the eye. Observing the angle fo the eye is an important part of the glaucoma eye examination, allowing the ophthalmologist to collect clues as to the type of glaucoma, and the type of treatments that would be most suitable for that particular eye. This examination is done by gently placing a special lens onto the sedated eye, much like a contact lens sits on the eye. This test provides information to the doctor about the inner structure of the drainage angle, whether it is closed, open or narrow, and may provide additional clues as to the subtype of glaucoma present in each particular eye, information that will greatly assist the glaucoma specialist in his/her work.
The tests described so far relate to the anterior part of the eye. However, in glaucoma the main damage occurs to the optic nerve, situated in the back of the eye. Therefore, to ascertain the presence and magnitude of any glaucoma present, the doctor may elect to occasionally examine also the inner parts of the eye.
Pupil dilatation
In order to examine the back of the eye the doctor instills special drops into the eye which dilate the pupil. These drops lead to temporary blurred vision (secondary to pupil dilation) which may last up to a few hours, especially noticeable for near vision (such as while reading). Dilated pupils also lead to discomfort in strong light (such as outdoors in the sun). It is recommended to refrain from driving while the pupils are dilated, since vision is somewhat blurred even for distance.
About 20-30 minutes after dilating drops have been placed into the eyes, the pupils grow large enough to enable the ophthalmologist to examine the retina, macula, and, in particular for glaucoma, the head of the optic nerve (also referred to as “optic nerve disc”.
Visual field test
 this is a computerized test performed to assess damage caused by glaucoma to the visual field. When we say ‘visual field’, what we mean is a term referring to everything that we see when looking at an object without moving our eyes. For example, when looking directly at a traffic light our peripheral visual field should enable us to also notice a car stopping beside us, noticed with our peripheral vision, which is a blurred image, but none the less informative. An accurate measurement of our visual field can reveal damage caused by glaucoma even in the very early stages of the disease, long before the patient can detect the earliest of symptoms. Regular testing of the visual field is a very sensitive way to follow progression of the disease in established glaucoma patients.
this is a computerized test performed to assess damage caused by glaucoma to the visual field. When we say ‘visual field’, what we mean is a term referring to everything that we see when looking at an object without moving our eyes. For example, when looking directly at a traffic light our peripheral visual field should enable us to also notice a car stopping beside us, noticed with our peripheral vision, which is a blurred image, but none the less informative. An accurate measurement of our visual field can reveal damage caused by glaucoma even in the very early stages of the disease, long before the patient can detect the earliest of symptoms. Regular testing of the visual field is a very sensitive way to follow progression of the disease in established glaucoma patients.
During the test the patient is asked to place his head on a chin rest, facing the device, and to look at a small constant light in front of him without moving his head or eyes. One eye is tested as the other is covered. While looking straight ahead, different lights are flashed from different directions and locations. The patient is asked to press a button every time he/she notices a light. This dim light is projected to different areas of the eye’s visual field, for brief periods of time. And in decreasing intensity until it is not noticeable at all. The test is structured such that some lights are easy to detect, some are very difficult to detect, and an equal number of light presentations are impossible to detect, since they are below the threshold of what even a healthy person can see. The purpose of this test is to determine the lowest intensity of light recognizable in various sections of the visual field, and from this information to construct a map of the visual field of that particular eye, on that particular day.
The advantage of this test is that it is computerized and is preformed in the same manner every time, and everywhere. The results are therefore far more standardized than when such tests were performed in the pre-computer era. This computerized test hence provides exact information that enables the doctor to determine whether the visual field is intact, abnormal, and if so, whether it has deteriorated since the last examination.
For a basic description of the visual field examination, go to ‘What is the Visual Field Test?’.
More information on interpretation of the visual field may be found in the chapter: ‘Deterioration of the visual field in glaucoma’.
Other tests for glaucoma- over the past few years, new methods for diagnosing glaucoma have been developed besides the time-honored tests described above. These are primarily imaging tests, using expensive, state of the art instruments that image and quantify the structure of the optic disc the front end of the optic nerve) as well as the thickness of the retinal nerve fiber layer, which is a measure of glaucomatous damage. These instruments are somewhat similar to a CT (computerized tomography) and ultrasound in their function, but use regular light instead of radiation or sound, to image the retina and nerve in order to measure any damage caused as a result of glaucoma.
To date, there are four types of instruments on the market which each functions using different physical principles. Presently they are used for both research and clinical purposes relating to diagnosis, progress and treatment of glaucoma. More recently, such imaging instruments have been put to use in the routine diagnosis as well as follow-up of established patients and it is likely that over the next few years we will see increased use of this approach in the clinic, providing more accurate information on the structural changes of the eye during the progression (or, hopefully, arrest) of glaucoma.
New technology is constantly being developed and tested to better diagnose and follow-up glaucoma. Some of this work is taking place at the Department of Ophthalmology at Rambam Health Care Campus, where clinical work is combined with clinical research towards perfecting the care of patients with complex eye conditions.