Patients who visit my clinic for the first time often ask me: “do I have glaucoma or perhaps not?”. Others who have already been diagnosed with glaucoma with certainty, might like to learn how their doctor came to this conclusion.
In this chapter, I will try to explain in detail how an ophthalmologist diagnoses whether or not a patient has glaucoma.
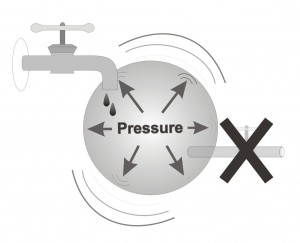
Glaucoma can be diagnosed, and characterized, via 3 different findings:1. High intraocular pressure
2. Visual field damage
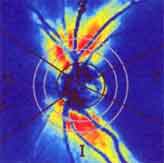
3. Damage to the optic nerve head (also called the optic disc)
Intra-ocular pressure is measured by the Ophthalmologist using a tonometer, which is an instrument that measures how high the pressure in the eye is. During this specific examination, the patient will see a blue light. Initially, eye drops will be placed into both eyes, eye drops which numb the eye and color the tears with a yellow tint. At the conclusion of the pressure measurement, the physician will have a reading for the intraocular pressure of the patients’ right and left eyes. The normal intraocular pressure may usually vary between 10-21 (average: 15). It is important to remember that even if the pressures are high only some of the time (not all readings, but only a portion of the readings) glaucoma can still develop and progress.
Note that some individuals have a sub-type of glaucoma which is called “normal-pressure glaucoma” (also called “low-pressure glaucoma”). Here, there is a situation in which the patient suffers from glaucoma although the eye pressure is never high (never found to be above 21). To try to understand this peculiar situation, we explain that in this certain individual, a pressure that is in the normal range is still too high for that eye, such that pressures need to be reduced to the low-normal range in order to stop or at least slow down the progression of the disease.
In addition to measuring the pressure, the doctor will also examine and evaluate the state of the optic nerve head. The optic nerve is situated in the back of the eye such that the doctor can examine it through the slit-lamp, while holding a lens. Usually, the doctor will dilate the patient’s pupils to see the nerve better, although the optic nerve can also be viewed through non-dilated pupils. The appearance of the optic nerve can teach an experienced ophthalmologist whether this eye has glaucoma. Occasionally there are borderline cases where it’s extremely difficult to say whether the nerve is healthy or else very early glaucoma is starting to develop.
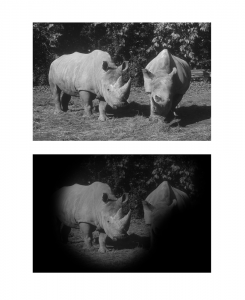
The third aspect of whether or not a patient has glaucoma, requires the doctor to send the patient to visual field testing. I said patient, but actually the individual may still be healthy. Only after visual field testing can we know for sure whether an eye is healthy or not. When performing a visual field test, small circles of light are projected at different points in space, in order to examine the visual field not only forward but also to the sides. The subject sits and places his (or her) face in front of a very large bowl, where the device will shine circular lights at different intensities, some of them very easy to identify and some very difficult to identify because they are very dimly illuminated lights. Every time the subject “sees the light” he/she should push a button that is held in the hand (somewhat like a TV’s remote-control). The machine will note when the subject saw the light and when he did not, and from that collective pool of information the device will create and print out a map of the visual field of that particular eye, on that particular day, such that your ophthalmologist will be able to diagnose whether this is a normal eye with a normal visual field or perhaps this eye does have glaucoma.
In order to diagnose glaucoma, your ophthalmologist will: measure the intraocular pressure and inspect the optic disc (the front end of the optic nerve), which resides in the far end of the eye (at the very back of the eye). Inspecting the optic disc provides information on the health of the entire optic nerve, but while the entire length of the optic nerve is hidden behind the eye (this is the nerve connecting the eye to the brain), the optic disc can be seen and examined using sophisticated instrumentation that ophthalmologists use in their clinic.
Hence, your ophthalmologist, basing his/her diagnosis on the measurement of intraocular pressure and optic nerve head (optic disc) appearance, can judge whether there is reasonable suspicion of glaucoma which requires visual field testing. Three pieces of information are crucial for diagnosing glaucoma: intraocular pressure, optic nerve head appearance and a printout of a visual field testing. At this point the eye doctor can usually provide his patient with an accurate answer whether or not they have glaucoma. Sometimes the ophthalmologist will conclude that the patient has “suspected glaucoma” which requires continued monitoring but still is not unequivocal enough to justify treatment. Of note, glaucoma usually affects both eyes, therefore if one eyeis found to have glaucoma, it is very likely that even though the other eye may not (yet) show any signs of this disease, it may do so some years down the road. An exception to this rule are those patients whose glaucoma is secondary to another process that occurs in the eye, patients who we say have “secondary glaucoma”. Processes leading to secondary glaucoma include surgery, severe injury to the eye, advanced diabetes that has damaged the eyes extensively, and a variety of other conditions that may indirectly result in increased intraocular pressure and lead to glaucoma. Most glaucoma patients have “primary glaucoma” – a glaucoma that happened without any underlying causes. Glaucoma in these patients, in the vast majority of cases, ultimately will harm both eyes. That’s why usually, when an ophthalmologist diagnoses glaucoma in only one of the eyes, he will also consider treating the presumably healthy eye (treatment that can be classified as preventative treatment).
In summary, glaucoma is diagnosed thorough a thorough eye examination performed by an experienced ophthalmologist. If the eye doctor suspects that glaucoma might be present, he/she will consider referring the patient to perform a visual field test. It is very important to note that glaucoma is a disease that has no symptoms, i.e. you do not feel anything wrong when you have glaucoma. Patients do not feel the increased eye pressure, do not feel the damage happening to the optic nerve head, and usually do not feel at all the impact of the disease on the visual field, except when the disease is in the very very advanced stages. Therefore, it is important to understand that the only way to diagnose glaucoma is by a routine eye examination performed by your ophthalmologist. It is of interest to note that the vast majority of people tested and found to have glaucoma, turn to the clinic because of other, unrelated, complaints, and just “by chance” happen to be diagnosed with glaucoma. In addition, some individuals show up in the ophthalmologist’s office because one of their first degree relatives (parents, brothers/sisters, children) have already been diagnosed with glaucoma, and because of a hereditary factor in this disease they have been instructed to be checked, and indeed in some of these individuals, glaucoma might be found.
It is important that all individuals over the age of 40 who are first-degree relatives of patients with glaucoma will have their eyes checked in order to deny (or confirm) the existence of this disease. All they have to do is schedule an eye examination, and tell the doctor: “My mother/sister/daughter has glaucoma, please check my eyes to rule out that I don’t have this condition as well”. Eevn if the eye exmination proves that they do not have glaucoma at this point in time, they will likely be told that they need to be monitored at perhaps yearly or bi-yearly intervals, to ascertain that no signs of glaucoma develop in the future. Should such signs ever be found, treatment would be initiated at a very early stage of the disease, treatment which will likely prevent the disease from ever becoming sight-threatening.