When ophthalmolgists use the term: ‘Diabetic retinopathy’, what they mean is that the retina (the seeing portion of the eye) has been affected by diabetes.
Diabetes is a relatively serious disorder which may jeopardize the health of many different organs in the body over the course of many years. It is worthwhile, perhaps, to take a moment and recall that until the advent of insulin not too many years ago, childhood diabetes was a disease that was impossible to treat.
Today, patients with insulin dependent diabetes mellitus, even if they acquired the disease at a very young age, can live an almost normal life with the help of insulin injections coupled with repeated blood tests aimed towards monitoring blood glucose levels. Those patients who do not require insulin, and have thus a milder form of the disease, can stabilize their blood sugar levels with the help of medications in the form of tablets as well as through a strict diet.
Thus, diabetes has turned into a chronic disease with which one can peacefully live a long and fulfilling life. If so, the problems that diabetic patients face today are the result of chronic changes that develop over years and decades of having this chronic disease. Of the very many problems that diabetes may cause, such as damage to extremities (for example, toes), to kidneys, to the heart, skin, blood vessels and more, one of the more devastating complications of diabetes mellitus involves damage to the retina. The importance of preventing this potential sight-threatening complication cannot be overstated.
Damage to the retina as a result of diabetes can lead to severe and irreversible decrease in vision. More so, it is important to realize that damage to the retina due to diabetes need not necessarily be a consequence of poor diabetic (sugar) control. Retinal damage may appear and possibly worsen, even in patients who are very well controlled in terms of their blood sugar levels. In other words: optimal control of diabetes is crucial, but it does not entirely ensure that retinal disease will not develop in the future. One characteristic of retinal involvement, in contrast to other complications of diabetes throughout the body, is that in many cases it is possible to treat, halt and even improve the retinal injury, provided that treatment is performed in a timely manner.
If so, what should we discuss with patients known to be diabetic?
First and foremost, any person known to suffer from diabetes should best be routinely followed by an ophthalmologist, often by his/her primary (health insurance appointed) ophthalmologist. The ophthalmologist will dilate the patient’s pupils in order to examine the retina and ascertain (or better yet, rule out) any effect of diabetes on the eye. Such exams are usually scheduled at intervals of every six months to a year.
It is unfortunate that many diabetics do not return for such routine visits performed by an ophthalmologist. If you, or a family member of yours, suffers from diabetes and does not routinely visit an ophthalmologist, it is very advisable to immediately recommend to him/her to put an end to this unfortunate situation! This is because the main reason for retinal damage in diabetics is due to neglect that results from the lack of medical follow-up when a patient does not regularly visit his/her ophthalmologist. It is not rare for a diabetic to be diagnosed with severe retinal damage and then realize that the patient had neglected to visit an ophthalmologist for quite a number of years.
In the event that the ophthalmologist finds changes that are a result of diabetes, he/she will decide if the damage is still early, such that it needs to be closely followed, or if it is more advanced, hence necessitating laser treatment of the retina. When such changes in the retina secondary to diabetes (usually damage to small blood vessels manifest as changes in the appearance of the retina as well as microscopic bleeding points) it is possible to treat the retina with a laser in order to slow down the development of further damage.
As I explained, despite the importance and necessity of proper blood sugar control in order to maintain a normal lifestyle with diabetes, blood sugar control does not always prevent the development of retinal damage. In those cases where retinal damage occurs, it often becomes necessary to treat using a laser, which is the main treatment currently available to slow the process of retinal damage. A diabetic patient crosses the threshold beyond which retinal damage requiring laser treatment occurs, that patient will be referred to an ophthalmologist, to receive treatment in which a laser serves to “extinguish” such areas of the retina that have been damaged as a result of diabetes. Such laser treatment, which is usually accomplished over the course of a few sessions, is capable of decreasing retinal deterioration and sometimes even assist in stabilizing the condition.
My advice to diabetics:
Diabetes is a chronic disease which accompanies a person throughout his/her lifetime. Millions are affected by this common disease. It is important to realize that dedicated timely treatment by an endocrinologist, as well as routine follow-up by an eye doctor can dramatically decrease the risk of this disease irreversibly damaging the retina.
I recommend and advise that every person who suffers from diabetes be sure to routinely follow-up with an ophthalmologist. In other words, schedule an eye-examination once every six months to a year, depending on what your eye-doctor recommends. The patient must know that if, God forbid, damage that requires intervention occurs, modern medicine has the ability to reduce the risk of further deterioration. Despite the fact that laser treatment does not help all cases equally, there is no doubt, and numerous studies have confirmed that, eyes that have been treated in a timely manner for diabetic retinopathy will suffer significantly less additional damage than similar eyes that have not been treated. Treated eyes will, on average, maintain better sight for years to come.
In summary
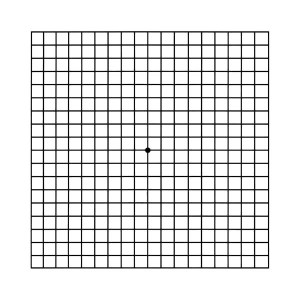
Many people belonging to the older population may eventually suffer from diabetes mellitus, a disease in which the body cannot utilize, metabolize, nor store sugar properly. Diabetes damages blood vessel walls throughout the body. These changes, in the eye, can lead to diseases such as cataract ,glaucoma and damage to eyesight as a result of injury to the blood vessels of the retina. Damage to these retinal blood vessels may lead to leakage of fluid or blood, thus damaging the inner eye, which is the retina, the seeing (film) part of the eye. This situation is known as diabetic retinopathy, a condition resulting in lack of clarity of vision, as well as distortion of the picture that the retina perceives and transmits to the brain, and in extreme cases may even lead to blindness.
Laser treatment is the most effective treatment for this condition. In the majority of cases this treatment does not succeed in restoring vision to its previous (pre-disease) clarity, but is effective in slowing further deterioration and worsening of the condition. Patients who suffer from diabetic retinopathy usually do not sense that something went wrong, and hence may not know that they are in need of laser treatment, since the damage is not perceived by the patient in the earlier stages of diabetic retinopathy. The best way to prevent retinal disease is through routine examinations by an ophthalmologist. It is advisable for diabetics to be examined at least once a year, or more frequently, as your treating ophthalmologist advises.