Am Fam Physician. 2004 1;70(1):155-156.
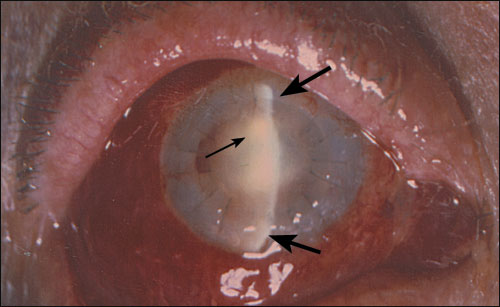
A patient presented to the emergency department with blurred vision, eye pain, and redness after corneal graft transplantation (Figure 1, note the radial black sutures). On physical examination, the patient had a painful red eye and decreased visual acuity. Slit-lamp examination (Figure 1, thick arrows show vertical line of slit-lamp illumination) revealed an intense inflammatory reaction in the anterior chamber (Figure 1, thin arrow shows inflammatory cells reflecting light).
Question
Based on the patient’s history and physical examination, which one of the following is the correct diagnosis?
- A. Acute angle-closure glaucoma.
- B. Bacterial conjunctivitis.
- C. Episcleritis.
- D. Endophthalmitis.
- E. Anterior uveitis.
Discussion
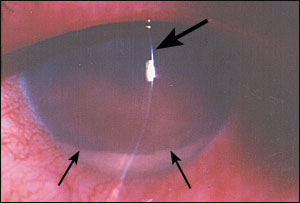
The answer is D: endophthalmitis. Bacterial endophthalmitis usually presents during the first week following intraocular surgery.1,2 The eye becomes red and painful, and symptoms rapidly worsen. Corneal haziness and vitreous clouding may develop, obscuring the red reflex on fundus examination. The anterior chamber develops a massive cellular and fibrinous reaction, which can precipitate as a whitish hypopyon(Figure 2, thin arrows show top margin of hypopyon; thick arrow shows slit-lamp illumination). Vision is markedly reduced. Intense ciliary and conjunctival hyperemia occurs, and diffuse eye swelling may occur, including the eyelids. Endophthalmitis is an acute emergency necessitating an urgent referral for intraocular injection of antibiotics, occasionally combined with vitrectomy surgery.3
Acute angle-closure glaucoma also may present with acute onset of pain, redness, and blurred vision. It is more common in the elderly. Acute closure typically occurs spontaneously but may be triggered by pharmacologic pupil dilation. It can lead to complete vision loss within 24 hours and is an emergency, necessitating urgent treatment with pressure-lowering medications combined with an iridectomy laser procedure (creating a hole in the iris with laser). It does not commonly occur in the postoperative period.
Selected Differential Diagnosis of Painful Red Eye After Surgery
| Condition | Characteristics |
| Acute angle-closure glaucoma | Shallow anterior chamber, elevated intraocular pressure, and edema of the corneal epithelium |
| Bacterial conjunctivitis | Purulent discharge, conjunctival redness, and edema of the ocular conjunctiva |
| Episcleritis | Sectorial or rarely diffuse redness caused by engorgement of episcleral vessels, large vessels seen beneath the conjunctiva |
| Endophthalmitis | Progressive and severe pain, decreased vision, eyelid swelling, chemosis, sometimes hypopyon, anterior chamber cells and flare, blurring of red reflex |
| Anterior uveitis | Red and painful eye, decreased vision, tearing, photophobia, cells and flare confined to the anterior chamber |
Bacterial conjunctivitis is characterized by conjunctival injection and purulent or mucopurulent discharge.4 Numerous microorganisms may induce bacterial conjunctivitis, so the course of the disease may vary from acute to chronic. Patients usually experience redness accompanied by discharge and stickiness of the eyelids, especially in the morning. Tearing and irritation may occur, but significant pain is uncommon. Conjunctivitis may be unilateral or bilateral.
Episcleritis is a descriptive term for any condition that causes inflammation of the episclera. Allergic causes are common and benign, but episcleritis also may be caused by more serious entities such as vasculitic diseases or systemic infections (e.g., syphilis or tuberculosis). Because the inflammation in episcleritis is limited to the outer layer of sclera, pain is not typical, and slit-lamp examination would not reveal any anterior chamber reaction.
Anterior uveitis, also referred to as iritis or iridocyclitis, is an inflammatory reaction affecting the anterior part of the eye.1,2 Anterior uveitis presents as acute inflammation characterized by intense redness, pain, photophobia, and reduced vision. Symptoms may develop over a period of hours to days. Slit-lamp examination findings include conjunctival hyperemia and an intense cellular reaction in the anterior chamber, which may result in the accumulation of a hypopyon. Uveitis may manifest as part of a systemic inflammatory condition (e.g., ankylosing spondylitis, inflammatory bowel disease).
ALBERTO J. MORALES, M.D.
EYTAN Z. BLUMENTHAL, M.D.
Hadassah University Hospital
Jerusalem, Israel 91120
REFERENCES
1. Duane TD, Tasman W, Jaeger EA. Duane’s clinical ophthalmology on CD-ROM. 2004 ed. Philadelphia: Lippincott Williams & Wilkins, 2004.
2. Jakobiec FA, Albert DM. Principles and practice of ophthalmology. 2d ed. Philadelphia: Saunders, 2000:CD-ROM.
3. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113:1479-96
4. Montzka D. The Wills Eye Hospital atlas of clinical ophthalmology CD-ROM. 2d ed. Philadelphia: Lippincott Williams & Wilkins, 2001.
