Kaiserman I, Anteby I, Chowers I, Blumenthal EZ, Kliers I, Pe’er J.
Ophthalmology. 2002 Jun;109(6):1137-41.
Department of Ophthalmology, Hadassah University Hospital, Jerusalem, Israel. Igork@cc.huji.ac.il
ABSTRACT:
PURPOSE: To analyze the postbrachytherapy ultrasonographic dynamics of uveal melanoma tumor height and internal reflectivity.
DESIGN: Prospective, comparative, observational case series.
PARTICIPANTS: One hundred forty-seven patients (147 eyes) with posterior uveal melanoma having a mean age of 61 years (range, 29-97 years) who were treated with Ruthenium 106 brachytherapy.
METHODS: Patients were followed-up with ultrasonography using both A and B modes of standardized echography every 6.7 +/- 0.3 months (mean +/- standard error of the mean) for a total of 1001 ultrasound examinations. On average, each patient was examined 5.8 times (range, 3-17 times). The echographic parameters included tumor base size, height, internal reflectivity, regularity, vascularity, and extra-scleral extension. To compare the response of tumors of different sizes, each tumor was standardized to its initial size at brachytherapy.
MAIN OUTCOME MEASURES: The dynamics of the tumor height and internal reflectivity.
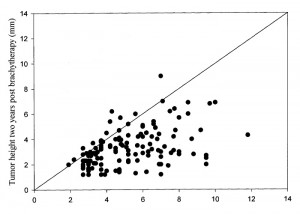
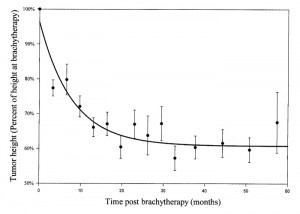
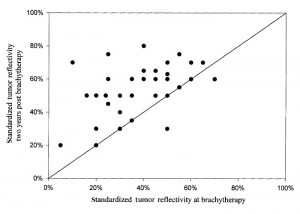
RESULTS: At the time of brachytherapy, the mean height of the tumors was 5.2 mm (range, 2.2-11.8 mm). After brachytherapy, 142 tumors (96.6%) responded by a decrease in height. The decrease in height was at an initial rate of approximately 3% per month. Most of the tumors did not regress entirely; rather, their height stabilized on a constant value (on average 61% of the initial height) after approximately 18 to 24 months. The decrease in height after brachytherapy was best fitted by the sum of a first order exponential decay and a constant (h = 61 + 35*e(-0.12t), in which t = time in months). The half-life of the decay was 5.8 months. Large tumors (>8 mm) had a faster initial decrease in height, and stabilized on a lower percentage of their initial height (50%) compared with small tumors (70%). Thus, the half-life of the height exponential decay was 5.3 months for small tumors (2-4 mm) and 3.3 months for the large tumors (>8 mm). Internal reflectivity increased from a mean of 40% before therapy to 70% after 2 years. The dynamics of the reflectivity were best fitted with the function: f = 45 + 24(1-e(-0.09t)). Larger tumors, which initially had lower internal reflectivity, presented with a slower increase in internal reflectivity (t() = 8.7 months) compared with smaller tumors (t(1/2) = 5 months).
CONCLUSIONS: The postbrachytherapy ultrasonographic dynamics of uveal melanomas resemble a function composed of the sum of a constant and a first order exponent, suggesting the possible existence of two components (cell populations), one unaffected by brachytherapy and the other a radiosensitive population that reacts to brachytherapy in an exponential decay. An exponential decay can imply that the postbrachytherapy death of each tumor cell is a stochastic Markovian process that is independent of the death of other tumor cells.
Figures from this article: